1-888-808-1845
Are you or a family member enrolled in Medicaid?
Welcome to the
Finger Lakes Region Social Care Network


We are here to support families and individuals with Medicaid in the Finger Lakes Region with access to essential services.
The Social Care Network brings together health care providers, mental health and substance use providers, professionals, care managers, and community organizations to offer extra support when it’s needed. By connecting medical care with everyday resources, we’re here to help Medicaid members people across the Finger Lakes region live healthier, more stable lives.
Our Mission
The mission of WeLinkCare by FLIPA is to improve the health and well-being of people by building an integrated network to connect them to the resources and support they need at the right time and right place.
- Allegany
- Cayuga
- Chemung
- Genesee
- Livingston
- Monroe
- Ontario
- Orleans
- Schuyler
- Seneca
- Steuben
- Wayne
- Wyoming
- Yates
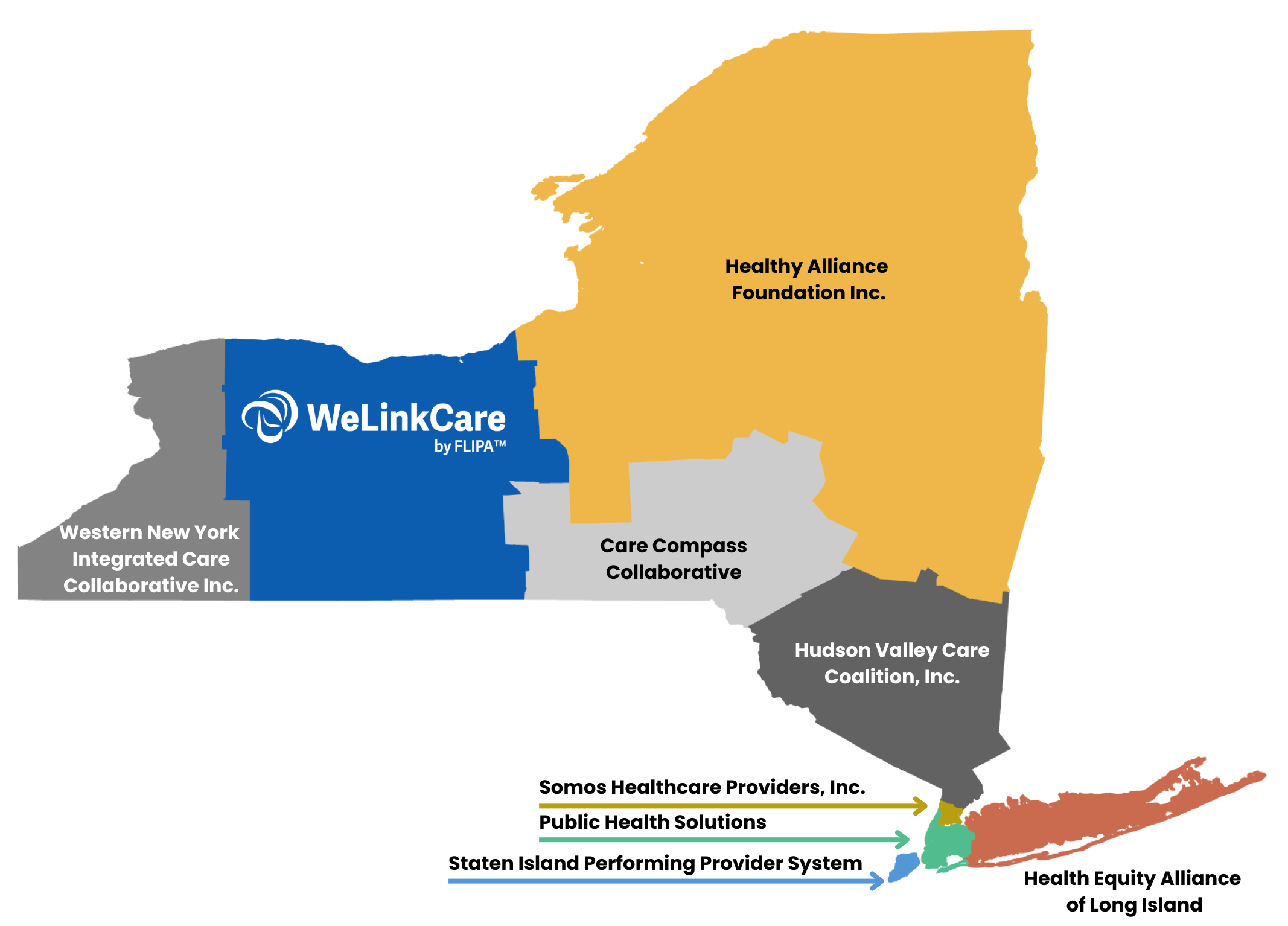
Not in one of these counties? Help is still available from one of the other Regional Social Care Networks.
What is WeLinkCare?
- WeLinkCare is the name of the Social Care Network in the Finger Lakes region.
- WeLinkCare is supported by Forward Leading IPA (FLIPA) who is NYS’ Social Care Network Lead Entity.
- WeLinkCare is a group of agencies committed and approved to provide Health Related Services Needs (HRSN) services to qualified Medicaid Members.
- WeLinkCare uses the FindHelp website to complete screenings, eligibility assessments, and connect Members to HRSNs.
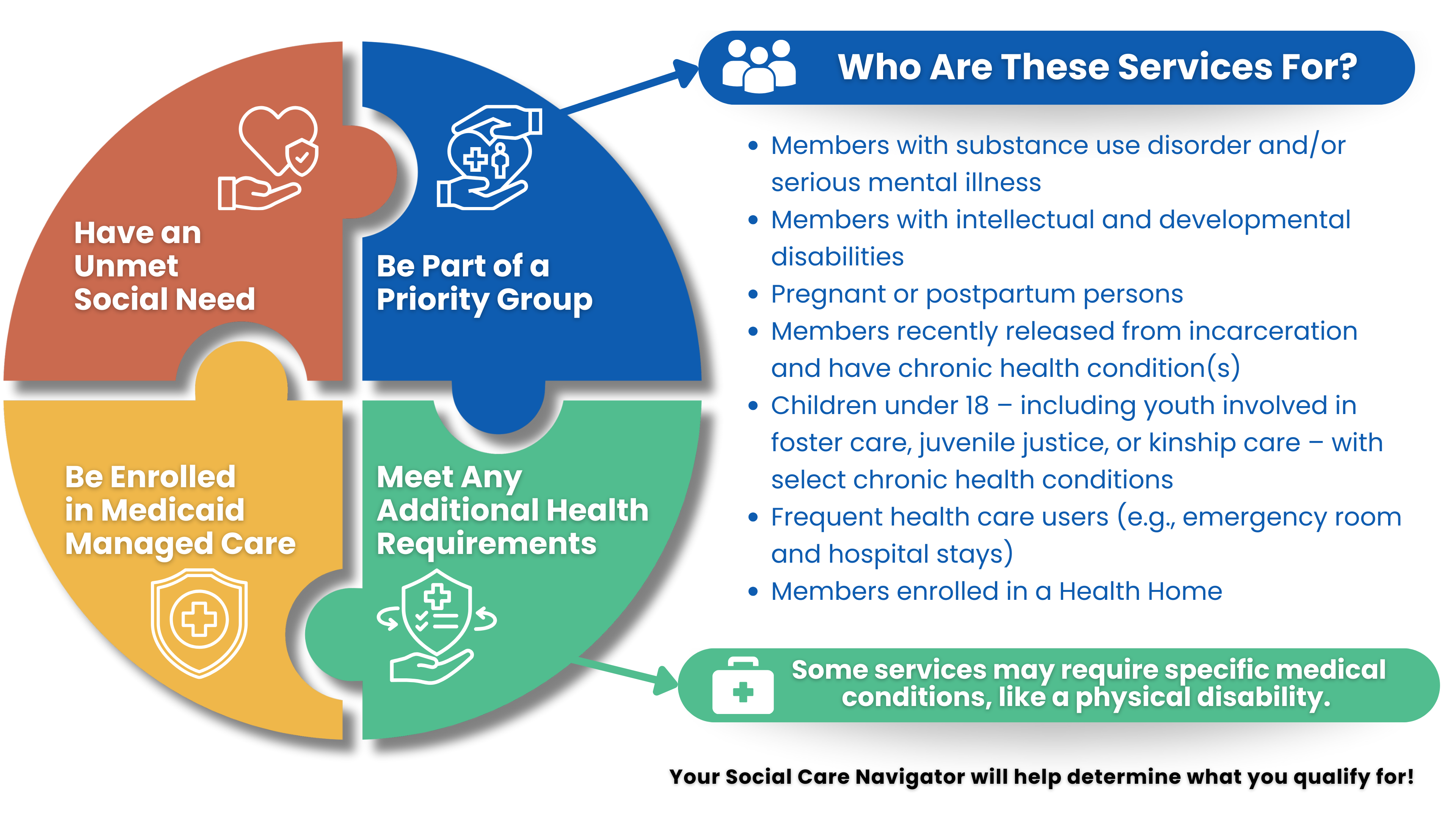
Am I eligible?
- WeLinkCare provides services to all Medicaid Members regardless of age.
- Active Medicaid enrollment is required.
- All Medicaid Members are qualified for and are encouraged to receive an HRSN screening every year and/or when they experience a major life event.
- eHRSN are provided to Members who are found eligible after completing an eligibility assessment.
- All Medicaid Members who consent can receive a screening to identified any Health Related Social Needs including transportation, food and nutrition, and housing.
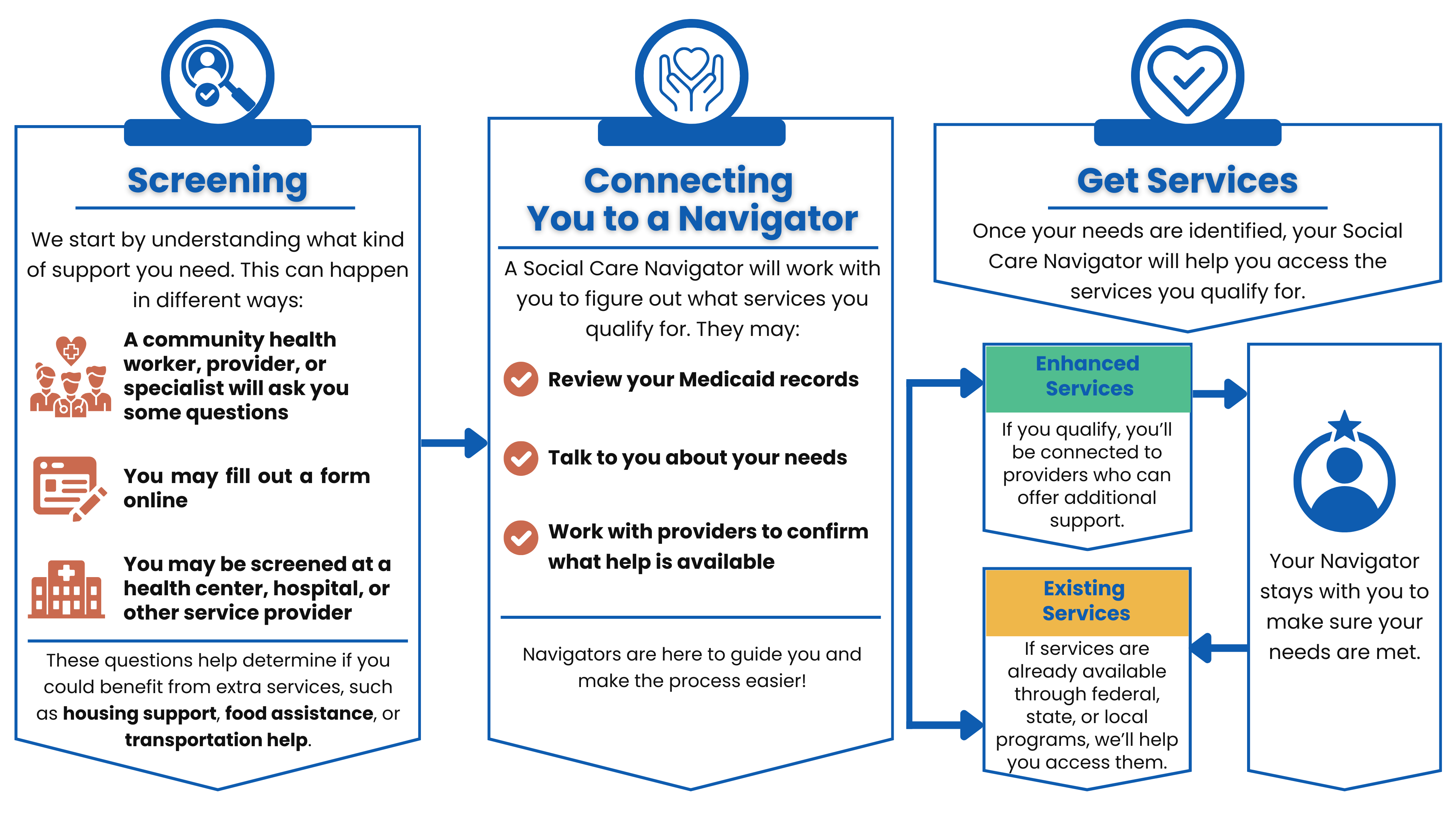
- Based on the outcome of the screening, Members may receive an eligibility assessment and/or support navigating to services based on need, preference, and availability.
- The eligibility assessment determines whether Members are eligible for navigation to existing health related social needs services provided by local, state, and federal programs and/or enhanced services delivered by We Link Care's partner community based organizations.
- Members who are eligible for enhanced services will be referred to enhanced services based on need, preference, and availability. Members receiving enhanced services will received additional care management support from a Navigator.
- WeLinkCare supports Members with determining their eligibility and need for HRSNs. Eligibility details can be found here.
What services are provided?
Screening, Navigation, standard, and enhanced HRSN services. HRSN services are those for Housing, Food, and Transportation needs.
Who provides the services?
- WeLinkCare’s Partner Agencies’ trained staff facilitate screening, navigation, and/or the health-related social needs services (HRSNs) to qualified Members.
- Screeners and/or Navigators complete the required screening, eligibility assessment, and assist with navigating standard and enhanced HRSNs and connecting members directly to the Housing, Food, and Transportation services.
Do I have to pay? How much does it cost?
- No, you do not need to pay. Services are provided free of charge to active Medicaid Members. You will not have to pay any money out of pocket. Services are billed to and paid for by Medicaid Fee for Service and Medicaid Managed Care to organizations providing services.
What if I have more questions?
If you have more questions, you can:
- Review the NYS’ Social Care Network page at Social Care Networks
- Email We Link Care at welinkcare@forwardleadingipa.org,
- Call 1-888-808-1845 (WeLinkCare)

Housing Support
Assistance with securing and maintaining stable housing.

Nutrition Support
Food assistance, counseling, and food prescriptions.

Transportation Services
Help with getting to and from health and social services.

If You Have Medicaid, We’re Here to Help
Whether have Medicaid through Fee-for-Service (FFS) or a Managed Care Plan (MMC), you may be eligible to be screened for health-related social needs (HRSN), like housing, food, or transportation. We can help connect you to local, state, and federal support programs.
If you're enrolled in a Managed Care Plan, you might also qualify for extra support through enhanced HRSN services. To get these extra services, you’ll need to meet certain eligibility requirements.
Medicaid Member Journey
The process to getting access to eligible services
Need Help? For more detailed information and to find resources near you, visit our SCN Find Help page. Here, you can access a wide range of services, from housing support to mental health resources, tailored to meet your individual needs.
To submit a self-screen regarding your health-related social care needs please fill out the Self Screen Form. This information will be shared with WeLinkCare and you will be contacted to discuss your responses and determine next steps.
Concerns?
If you are a Medicaid Member who has a concern or complaint, please contact us.
Ready to get involved or learn more?
Contact Us
Reach out to us today at welinkcare@forwardleadingipa.org or call
